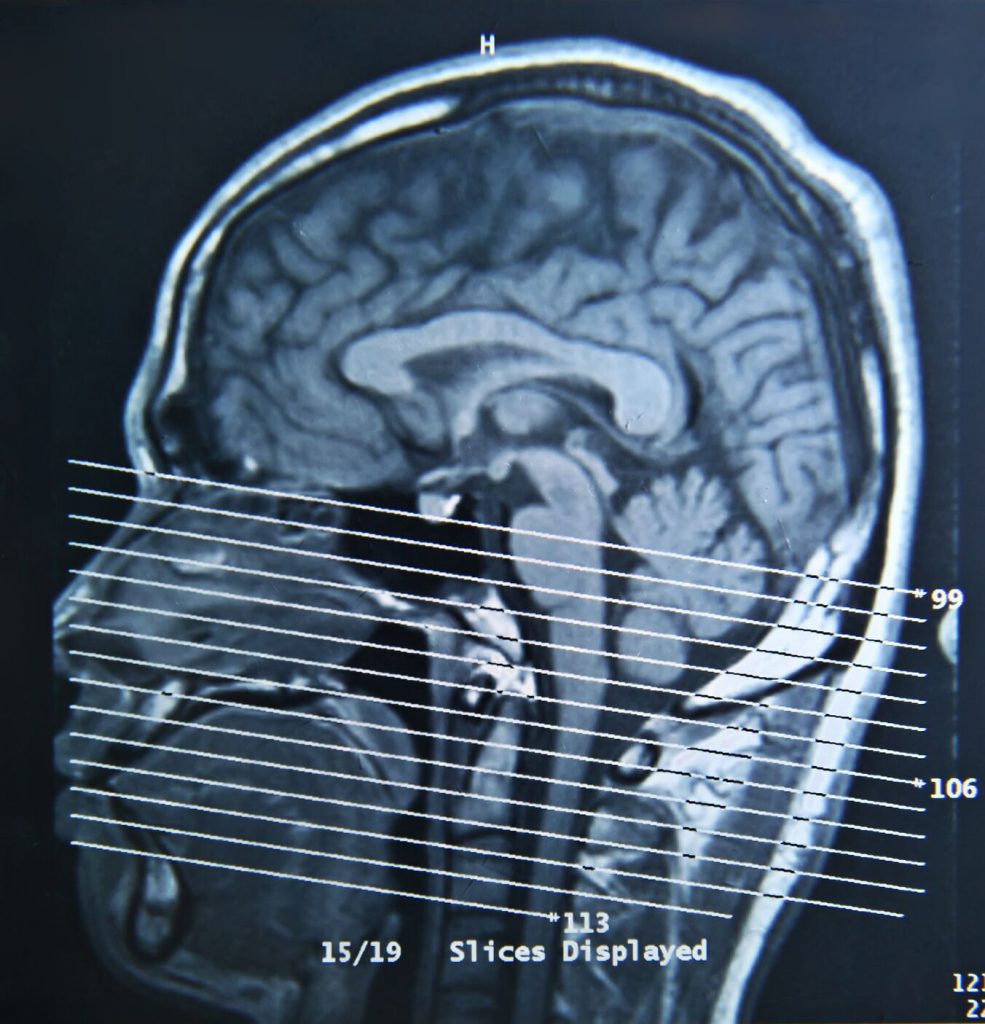
John Hopkins researchers have shown that non-invasive CT angiograms are more effective at detecting clogged coronary arteries than exercise stress tests. Around 15 million Americans visit physicians each year with symptoms of a clogged artery. Chest pain, shortness of breath and fatigue often warrant further testing to spot any blockages. Cardiologists typically rely on a stress test that measures blood flow after a patient walks on a treadmill. American Heart Association guidelines currently call for this test when patients show signs of coronary artery disease. The new study indicates that CT angiograms may be a better testing method due to lower radiation levels, higher accuracy and comparable cost.
The gold standard for detecting clogged arteries remains an invasive cardiac angiography. This test involves threading a catheter into a patient’s heart blood vessels. It’s a process that carries certain risks, so cardiologists utilize an initial “gatekeeper” test to identify the people most likely to benefit from it. The John Hopkins study shows that stress tests only correctly identify blockages in 6 out of 10 people. Comparatively, CT scans accurately spotted blockages in 9 out of 10 patients.
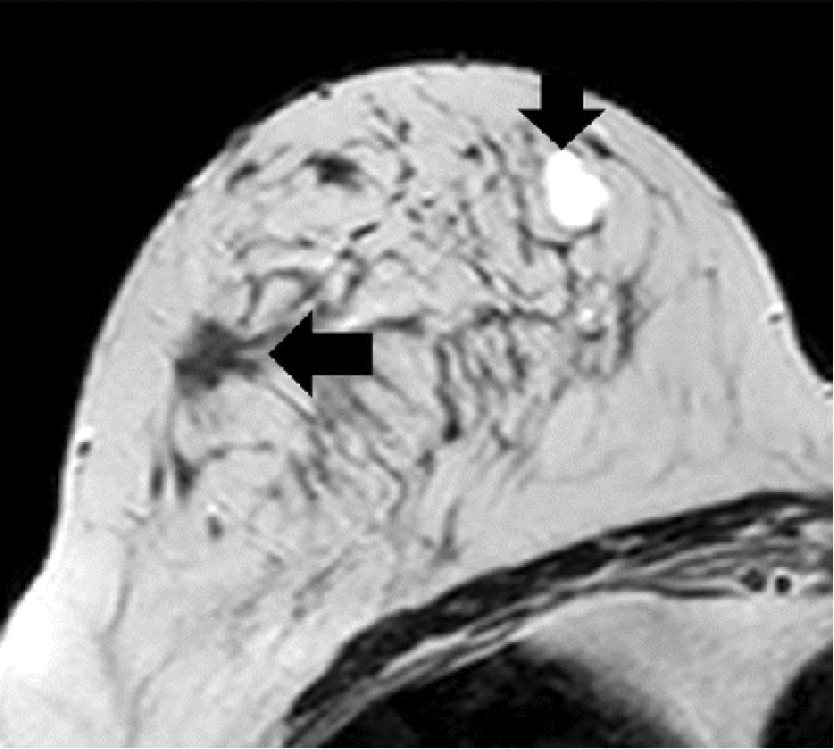
Participants of the study underwent all three testing methods, providing a direct comparison of the effectiveness of each. For CT angiograms, clinicians inject dye into a patient’s circulation to visualize the arteries. The test spots blockages caused by fatty buildups or clots in the interior of arteries. Clinicians have shied away from this process in the past due to limited evidence of its efficacy. The recent study examined 391 patients in 16 hospitals and eight countries. It was the largest study of its kind to date.
The researchers hope that the results show clinicians that CT angiograms are a more accurate alternative than the widely used stress tests. Both tests provide a first-line diagnosis before an invasive cardiac angiography. The unprecedented scale of the study gives cardiologists solid evidence to support CT scanning. For patients concerned about blocked arteries, the results are promising. A near-perfect diagnosis rate seems more realistic than ever before.