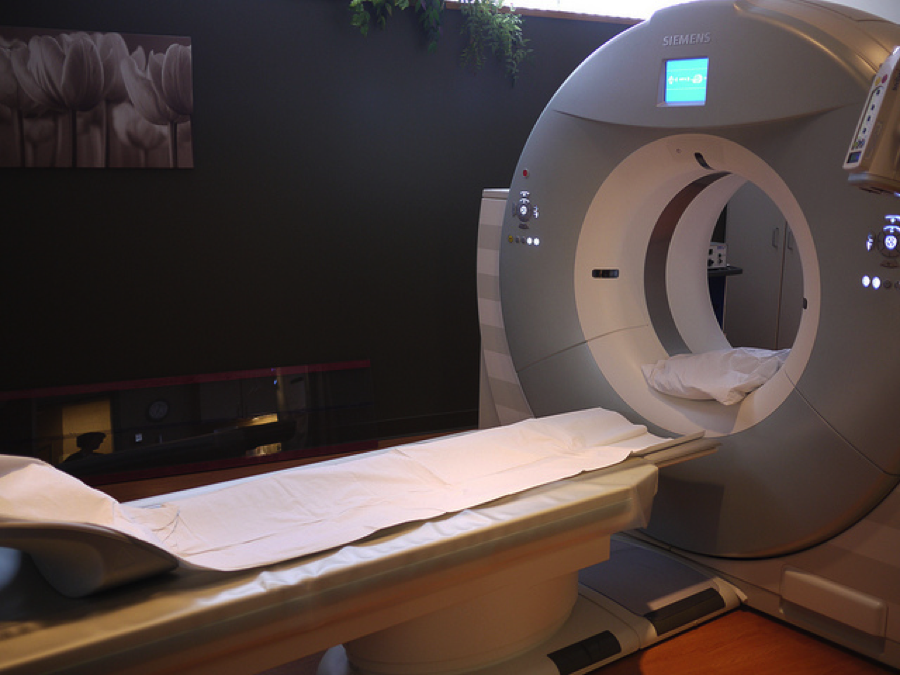
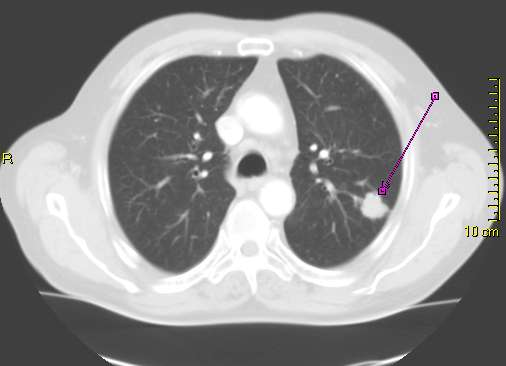
Children and young adults with right lower quadrant (RLQ) pain may benefit from an MRI diagnosis, according to a new study published in Radiology. A University of Arizona team determined the accuracy of unenhanced MR imaging for patients in the retrospective study. In all, the researchers examined imaging from 403 patients with an age range of 3-49 who experienced RLQ pain and received an MRI. The team suspected that intravenous or oral contrast methods were unnecessary with the use of an MRI diagnosis.
To learn more about MRI accuracy, the team looked at clinical records that documented MRI room time as well as prospective image interpretations. While some of the patients suffered from appendicitis, others were experiencing other types of abdominal pain. Attaining information for patient outcomes was essential for the study. The team was able to collect final results for patients with documentation including surgical results, telephone follow-ups, medical records and expert panel assessments.
Gathering patient data was important, but the results mattered most. The study revealed that the average MRI room time was 14 minutes. Among the 403 patients, 67 tested positive for acute appendicitis, while 336 had negative results. The MRIs had 97% sensitivity and 99.4% specificity. 51.5% of the patients were diagnosed with an illness other than appendicitis. This high degree of accuracy led the researchers to conclude that MRIs are an effective way to evaluate and diagnose RLQ pain.